Learning about keratoconus
What is Keratoconus ? |
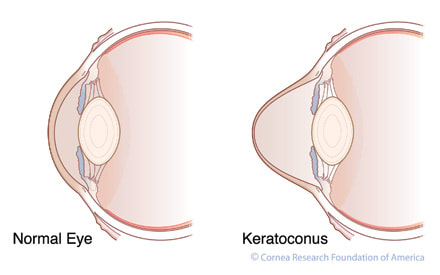
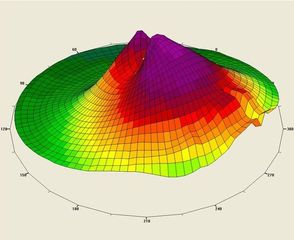
Keratoconus is a progressive eye disease in which the normally round cornea thins and begins to lose its natural shape and bulge into a cone. This cone shape distorts a persons sight leading to a loss of vision that cannot always be corrected with spectacles alone. The degree of Keratoconus can vary from having no effect on the person's vision up to limiting everyday tasks such as driving.
Progression can vary from person to person and monitoring is important to prevent further deterioration. These images give an impression of what someone with keratoconus may see compared to someone with normal vision. |
The earliest signs of keratoconus are usually blurred vision and frequent changes in eye glass prescription or vision that cannot be corrected with glasses. Symptoms of keratoconus generally begin in late teenage years or early twenties, but can start at any time.
Other symptoms include:
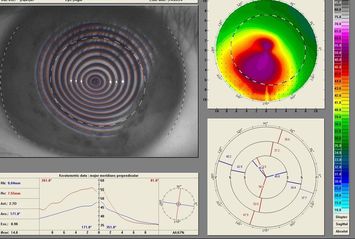
Keratoconus requires a diagnosis from a through eye test with an optometrist. At the Valley Plaza Optometrist we can detect Keratoconus using a corneal topographer as well as examining your corneal health with a special microscope.
Other symptoms include:
- Increased light sensitivity
- Difficulty driving at night
- A halo around lights and ghosting (especially at night)
- Eye strain
- Headaches and general eye pain
- Eye irritation, excessive eye rubbing
Keratoconus requires a diagnosis from a through eye test with an optometrist. At the Valley Plaza Optometrist we can detect Keratoconus using a corneal topographer as well as examining your corneal health with a special microscope.
|
Keratoconus can usually be diagnosed with a regular eye examination. The classic signs of keratoconus that the optometrist will see when examining your eyes may include:
The optometrist will also measure the curvature of the cornea. This is done by:
|
Options For The Keratoconic Patient

For many of our Keratoconic patients corection with spectacles or regular soft contact lenses will be enough to achieve a good quality of life. However for many others they will still see blurred vision and night haloes that prevent them from driving or performing normal daily tasks.
For these people they will need to be fitted with a special type of contact lens known as an RGP (Rigid Gas Permeable) lens. This effectively replaces their distorted corneal surface with a new optical surface free of distortion allowing good clear vision . These are worn daily instead of spectacles and removed before sleep. They provide incredible freedom to those who would otherwise need surgery.
RGPs lenses are not without their challenges. Problems associated with many RGP fits include:
For these people they will need to be fitted with a special type of contact lens known as an RGP (Rigid Gas Permeable) lens. This effectively replaces their distorted corneal surface with a new optical surface free of distortion allowing good clear vision . These are worn daily instead of spectacles and removed before sleep. They provide incredible freedom to those who would otherwise need surgery.
RGPs lenses are not without their challenges. Problems associated with many RGP fits include:
- Initial discomfort - in particular distraction with lens interaction with upper lid.
- Discomfort with any foreign body trapped under the lens making lenses hard to use in dirty or dusty environments
- Tendency for lenses to fall out without warning during sport or if the eyes are rubbed excessively. If lost lenses are expensive to replace.
New Technology Provides Hope For Those Struggling With Keratoconus
|
Well-fitted Mini-Scleral Lens on Patient with Keratoconus
Keratoconic With Fluorescein Dye Used in Fitting Process
|
For these reasons we have been successfully using a newer lens design that eliminates all of these problems. These Semi-Scleral lenses are a larger size that sits neatly under the lids. This eliminates many of the problems experienced by those unable to adapt to the discomfort normally associated RGP lenses.
If you have had problems with Keratoconic lenses before you should consider this new technology because of:
Getting fitted for your keratoconus is as simple as making an appointment to discuss your options. After an initial exam we will take special measurements of your corneal shape to determine the best lens course for you. Contact lens fitting can take a few weeks of fitting and adjustment during which time we will show you all you need to know about handling and cleaning lenses. |
So if you have had problems with RPG lenses in the past and do not want to give up on good vision why not come and see us to review your options. All assessments for Keratoconus can be bulk-billed to medicare.